TOUCHPOINTS AND NURSE SENSITIVE INDICATORS: EXPLORING OPPORTUNITIES to IDENTIFY NURSING’S CONTRIBUTION to QUALITY IN PRIMARY CARE
By Honor Carroll Martin, RN, MS, NE-BC, CHCQM, FABQAURP
HCQM Certified: 9/14/1997
 BACKGROUND
BACKGROUND
As patients and healthcare professionals, we all can appreciate the roles that nurses fulfill in supporting clinical systems. Patient outreach and teaching, assisting providers, overseeing quality audits, conducting telephonic and virtual triage, and responding to patients’ urgent care needs, are just a few of the many ways in which the primary care environment is enriched through nursing practice. The roles of Clinical Care Coordination and Transitional Care Coordination, both of which have been identified as important navigational elements in healthcare and which have become more developed in the past ten years, are considered to be best performed by registered nurses in primary care settings. (American Nurses Association: The Value of Nursing Care Coordination: A White Paper, 6/12: p. 6.)
As reimbursement models continue to evolve over time and sustain an ever-growing registry of quality indicators, the caliber of practice required to identify excellence in the primary care environment also expands. Batiste-Brown (2023) states that true clinical effectiveness will require nursing leaders to move away from historical training and roles and look toward new ways to employ resources. The mining and analytics required for accurately reporting evidence of quality supports the need to develop new ways to coordinate the patient experience. This article will explore ways in which the practice contributions of nurses in the primary care environment are linked to quality industry standards as well as to Nurse Sensitive Indicators (NSIs).
ASSESSING THE CONTRIBUTIONS OF REGISTERED NURSES IN THE PRIMARY CARE ENVIRONMENT
Unfortunately, in many clinics and medical centers across the country, staffing with registered nurses is sparse at best. Salaries and benefits that would ordinarily be needed to attract exceptional candidates frequently come at too high a price for many employers. However, the additional financial outlay for hiring registered nurses in primary care settings, and ultimately for providing them with the tools necessary to progress to executive leadership, can potentially result in positive change for patient populations, providers, and operational reimbursement.
As we look to incorporate lessons learned from the Covid pandemic and the change it has already brought to healthcare in this country, we might explore ways to further build structure, process, and outcome validation through nursing’s contribution to that changing environment. Nurse-sensitive indicators (NSIs) are a reflection of the value which nurses bring to the primary care setting. They embrace clinical support, influence improvement in patient literacy and health system navigation, and ultimately can positively improve evidence-based results. Dish and Finis (2022) state that nurses provide measurable quantitative and qualitative value beyond the number of patients cared for or associated costs. As the health care professional who most often can establish effective contact with a patient outside of provider office visits, registered nurses engage patients in a process that begins with advancing patient literacy and health system navigation to providing necessity for preventive and diagnostic screening. Nurses can respond to patient questions regarding chronic disease management, often allaying fears, while at the same time establishing a basis for patient goal-setting.
Gordon and Gadbois (2018) predict that insurance expansions under the ACA will require 52,000 additional primary care physicians by 2025. Recruitment to fill this enormous number of vacancies will come at a staggering cost. Most primary care clinics that serve the poor do not produce robust financial earnings. Consequently, any opportunity to improve the bottom line is not only desirable but in some cases essential to address the needs of those living in poverty or disenfranchisement. Financial status in these clinics is often influenced by a number of stressors, each of which can create hardship, but reimbursement rates are frequently the overriding factor (Gordon and Gadbois, 2018). This is even more evident in primary care centers that are contracted through a cluster of financial reimbursement models or government reporting structures. Managed care companies have exchanged many traditional primary care contracts in recent years with shared risk agreements which are directed at keeping patients healthier but require achievement of high levels of imposed quality indicator compliance to produce improved reimbursement. Patients are encouraged to seek preventive care more readily which can improve their overall health (May and Start, 2021). Whatever savings may result, though, are reliant upon the identification of opportunities to collect quality indicator data as thoroughly and efficiently as possible. This takes time and clinical expertise. Workforce sustainability planning for primary care in the future will need to include the creation of new roles for registered nurses that not only support potential provider shortage deficits through nursing’s performance of more specialized clinical tasks, but also the creation of nurse specialist roles in identifying, connecting, applying, and analyzing clinical quality indicators in nursing practice. This will need to take place within a growing technical and virtual information repository.
REGISTERED NURSES, NSIs, AND QUALITY DATA COLLECTION
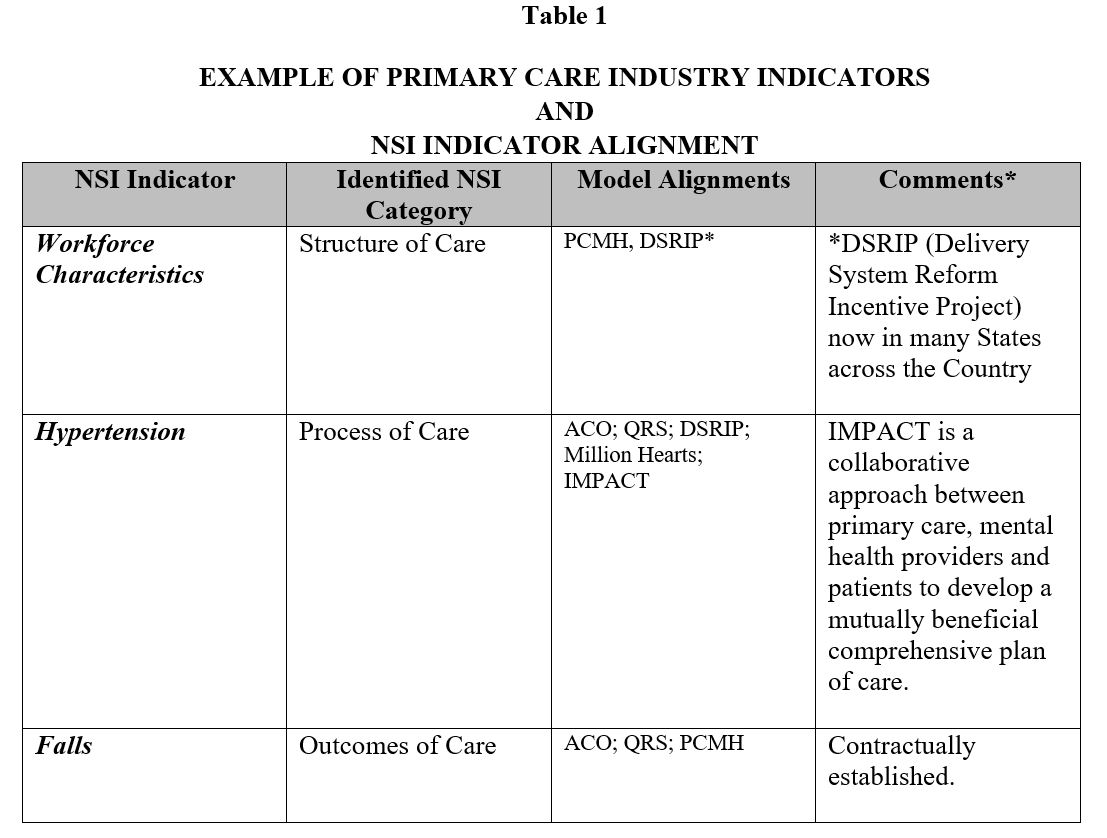
Demonstrating the value of nurses collecting NSI information, which frequently aligns with healthcare quality industry indicators, can lend validation to the important role nurses contribute to the gathering process (May and Start, 2021). An example of how NSIs align with indicators which the payment models and government mandates require, and which can provide positive reimbursement streams, are also important for budgeting and staffing. May and Start point to the shift from episodic disease treatment to disease prevention as a critical need in transforming primary care. But this shift may also be critical in supporting better reimbursement. The mapping of specific clinical intervention gleaned through the cross-referencing of primary care industry indicators and their alignment with nurse-sensitive indicators can also be instrumental in the development of policies that focus not only on the integrity of the collection of data, but also the follow-up that can occur through nursing intervention. In short, policy drives process and process drives practice. Furthermore, when it comes to clinical review and assessment, registered nurses offer a depth of expertise that derives from their academic nursing programs and their experience. Care coordination and transitioning of care flow naturally from the identification of links to industry quality standards, but both pathways have the potential to create significant financial and operational value through nursing intervention. An example of this alignment can be viewed in Table 1.
NURSING TOUCHPOINTS AND QUALITY INDICATOR DATA
NSIs define elements of quality that are linked to nursing process, including evaluation, clinical review and analysis, and defining strategic clinical actions based on medical evidence. As such, they can illustrate specificity in nursing practice. Similarly, touchpoints can identify elements of quality as they relate to nursing intervention. In both cases, a relationship exists between any quality indicator common to both and a process that connects the indicator with an outcome. Sudbury-Riley et al. (2020) describe touchpoints as representing “any point of contact between a service user and any aspect of the service. Touchpoints are also clusters of experiential elements that foster product or service experiences” (p. 4). Nurse touchpoints, categorized here as Direct and Indirect, can be defined as the incidents in daily nursing practice that involve a registered nurse’s interactions or intervention with a patient, or a staff member regarding a patient, and the nurse’s interactions through subsequent practice activity relative to critical patient information or tasks related to patient care. This information might be shared with a provider, with a clinical team coordinating care for the patient, or it may be entered into the patient’s record. Touchpoints can be defined, therefore, as the contributions nurses make on behalf of a patient with regard to time, nursing practice, and clinical documentation.
Direct Touchpoints in primary care include activities such as the review of a patient’s medications in preparation for a medical visit, the review of lab work, consultations and care plans from specialists that need to be communicated to patients, and the acknowledgement of that communication entered by the nurse into the patient’s medical record. It is also the care coordination provided for a patient which may involve scheduling of diagnostic testing or procedures, educating a patient on medication changes or providing information on the rationale for a provider’s order. In transitional care, patient contact by the nurse post-discharge ensures that the patient is scheduled for follow-up care within two-to-three days, and any environmental changes required for safety and discharge to home are completed. Notification to the family regarding the patient’s care and equipment needs are also important parts of the transitional care plan. Indirect Touchpoints in primary care can be defined as those communications which are conveyed to healthcare staff in conjunction with specific directions for completion. In this case, touchpoints provided by nursing leaders or managers could include directing the scheduling of a patient for an urgent care visit, completing any new patient directives required by the clinic or medical center for a patient’s primary care or follow-up visit, or other mandates deemed necessary for patient comfort or safety.
Any time a nurse contacts a patient, completes an entry in a patient chart, or provides documentation on a specific health event derived from a triage episode, is a touchpoint and should be considered a quality process element. Touchpoints can be defined in nursing practice as part of nursing’s contribution to patient care and they can be calculated in terms of time expended by the nurse as well as the reporting of evidence-based results. In addition, the gathering of information by the nurse to meet external or governmental quality mandates such as HEDIS (Health Effectiveness Data Information Set), PCMH (patient-centered medical home), or CMS (Centers for Medicare & Medicaid Services) reporting are direct touchpoints and are enhanced through a nurse’s clinical knowledge. A registered nurse’s identification and reporting of quality indicator information within the context of nursing practice lends a high level of clinical integrity and accuracy to measurement and analytics. This can be validated through comparisons between electronic medical record (EMR) reports and nurse-audited reports. Frequently the nurse-audited reports reflect indicators difficult to identify through a technology drop since key words used in the descriptive programming may not completely define the required medical outcome necessary to meet the reporting requirements.
The advent of value-based payment and pay-for-performance health plan models over the past decade, as well as the contractually required assumption of financial risk for provider groups now common in health plan management contracts, have challenged health care professionals to embrace a new level of surveillance. The ability to measure quality performance through technology systems, sculpted by tailored indicator algorithms, is now part of a day-to-day data collection and review process in many primary care centers. For their part, EMR systems have evolved over time to meet the information technology demand of medical practices and government-mandated reporting. These systems can now house and report on numerous categories of data in their repositories, and reports can be configured to collect information through a myriad of features. These reports can calculate units of time spent for chart analysis, patient guest relations, or staff data entry through sophisticated audit systems. EMRs can also demonstrate the symbiosis that exists through comparative reports that reference EMR and nurse reviews and compile specific quality elements as well as quantify nursing’s contribution in terms of time expended in clinical activities.
CALCULATING NSI VALUE AND CLINICAL QUALITY PERFORMANCE
There are many who would argue that the influence of nurses in primary care settings encompasses a host of variables which really cannot be calculated. However, the time spent by the nurse through teaching, review, and communication of clinical information to patients can and should be counted as contributory to a patient’s health and wellness. These nursing activities can point to improved patient visits where specific health issues can be more comfortably discussed, goals can be established, and preventive care can be reviewed in the presence of the nurse, provider, and health care team. From the standpoint of clinical preparation, these activities provide an enhanced contribution to both the NSI and industry quality indicator data collection process.
SUMMARY
Registered nurses bring a valuable level of clinical expertise to the gathering of quality indicator collection, whether identifying/collecting industry required quality markers as part of a pay-for-performance reporting schematic or through identified NSI data collection. These tasks are enhanced through direct and indirect touchpoints and they reflect a complementary process which registered nurses are exceptionally well-equipped to provide through their expertise and knowledge base. Through reporting and analysis, nurses have the ability to build patient health profiles. They bring important communication ties to their patients, especially those with varying cognitive abilities. Nurses identify patient issues in concert with their day-to-day responsibilities and manage multi-functional environments, making them exceptionally valuable as clinical support for primary care and ancillary providers. Their added expertise in extracting industry quality markers and nurse-sensitive indicators for reporting purposes make registered nurses even more valuable from the perspective of harvesting information to supporting financial operations for their primary care employers. These tasks can also reduce the time primary care providers spend in completing required record entry tasks, thus enabling them to afford more time to more comprehensive patient clinical oversight.
The contributions of nurses to nursing practice are a powerful argument to increase registered nurse staffing, and they also underscore the variety and depth of skills needed to support positive patient experiences. The ability of nurses to reach patients both clinically and emotionally through enhanced communication provides the basis for trusting and satisfying relationships. These activities encourage improvement in patient literacy and health care consumerism.
The consideration of nurse touchpoints creates a method to calculate units of time afforded to patient interactions and nursing practice activities during the course of a day. EMR systems can be used to calculate nursing time spent on patient record review as well as indicator harvesting for cyclic mandated reporting. The dedication of time that nurses contribute through nursing clinical support tasks and communication with patients can provide a calculable metric with which to review their efficacy as employees and their value relative to patient care. Retrieving evidence-based data from nursing interventions, and applying nurse-sensitive indicator architecture to identify the measurement of quality through a patient’s positive achievement of goals, are directly related to that nursing intervention. Similarly, patients’ potential improvement in recommended preventive screening through longitudinal profiling can provide validation of successful nursing-patient interaction and follow-through.
Looking to the future, nursing positions built on touchpoint interventions, direct and indirect, offer a new look at how clinical intervention can support quality indicator gathering for nurse-sensitive indicators and required health care industry indicators alike. These interventions also have the potential to create new specialty certification areas for registered nurses which can enhance primary care, promote heightened awareness for the value of nursing practice, and provide workforce opportunities for registered nurses in primary care that may supplement the shortage of nurse staffing for the next generation.
REFERENCES
American Nurses Association. (June 2013). The value of nursing care coordination: a
white paper. doi: 10.1016/j.outlook.2003.10.006
Batiste-Brown, Q. (March 2023). Advancing clinical practice in ambulatory care: the role of nursing
leadership. The Voice of Nursing Leadership, p. 17.
Disch, J & Finis, N. (2022). Rethinking nursing productivity: a review of the
literature and interviews with thought leaders. Nursing Economics, 40(2), pp. 61,
64-65.
Gordon, S.H. & Gadbois, E.A. et al. (2018). Quality perspectives of primary care
providers who treat medical managed care patients. BMH Health Services
Research. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6150984
May, N & Start, R. (2021, July 6). RN value across the continuum: the evolution of
ambulatory nurse-sensitive indicators. The Voice of Nursing Leadership.
https://www.aonl.org
Sudbury-Riley, L, et al. (2020). Introducing the trajectory touchpoint technique: a
systematic methodology for capturing the service experiencing of palliative care patients
and their families. BCM Palliative Care, pp. 1-13.
doi: 10.1186/s12904-020-00612-2